Intracranial pressure (ICP) refers to the pressure inside the skull and can increase due to head injuries, bleeding or tumor growth in the brain. A elevated ICP can cause potential damage to the brain tissues and requires close monitoring. Intracranial pressure monitoring devices are crucial for neurosurgeons to continuously track the ICP levels and detect any sudden changes which enables timely clinical intervention. Conditions like traumatic brain injury, subarachnoid hemorrhage and hydrocephalus often warrant ICP monitoring for optimal management and improved patient outcomes.
Types of Intracranial Pressure Monitoring Systems
The two major techniques used for intracranial pressure monitoring are invasive methods involving placement of monitoring devices inside the brain and non-invasive methods without implantation of intracranial pressure monitoring devices. Invasive ICP monitors include external ventricular drain, intraparenchymal monitor and subdural screw. The external ventricular drain is placed into the ventricle to drain excess cerebrospinal fluid while intraparenchymal monitors are directly implanted into the brain parenchyma. Non-invasive methods such as tympanic membrane displacements provide indirect measure of ICP but cannot match the accuracy of invasive monitors.
External ventricular drain remains the gold standard invasive method and is inserted through a burr hole into the ventricle. The device is connected to both a pressure transducer and an external drainage system. Intraparenchymal monitors like neuron sensor consist of a strain gauge sensor at the tip which is implanted directly into the brain tissue providing continuous numeric ICP readout. Subdural screw ICP monitor screws into the skull and has a strain gauge transducer at its outer end for ICP measurements.
Advantages of Invasive ICP Monitoring Systems
Invasive monitors offer highest accuracy by direct measurement of pressure within the brain parenchyma or ventricles. Real-time continuous monitoring is possible for durations ranging from days to months based on the clinical need. Immediate pressure values and waveform patterns aid neurosurgeons in timely diagnosis and treatment decisions. Placement of monitors is also minimally invasive involving small burr holes with relative ease of implantation. Possibility of cerebrospinal fluid drainage with external ventricular drain helps maintain normal ICP levels in conditions like hydrocephalus.
Challenges and New Advancements
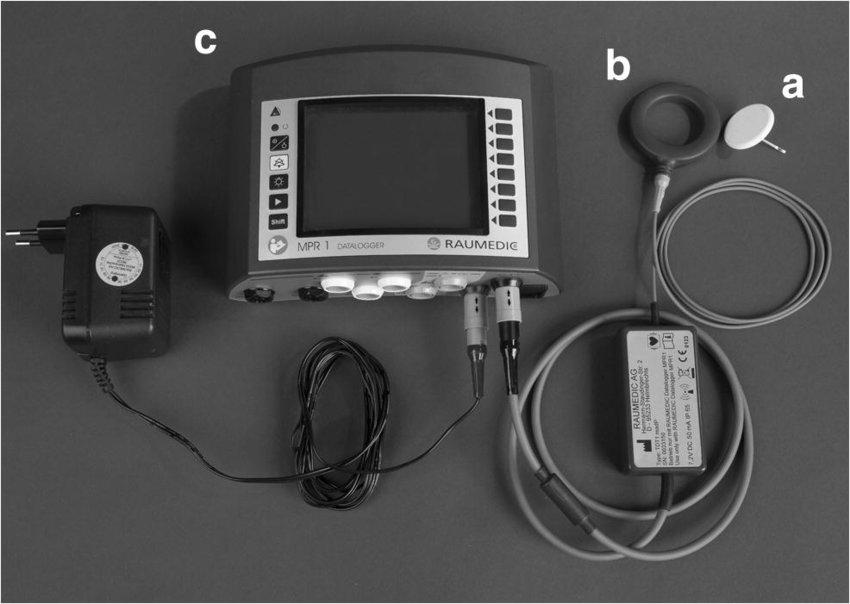
Despite advantages, complications like hemorrhage, infection and device malfunctions are challenges with invasive methods. Non-invasive techniques cannot substitute the accuracy of direct ICP reading but avoid risks of implantation. Novel implantable devices are integrated with additional sensors for multi-parametric monitoring. Wireless technology enabled ambulatory monitoring systems have increased patient mobility. Miniaturized flexible monitors are undergoing clinical trials. Advancement of biocompatible materials and calibration techniques will further enhance safety, accuracy and usability of intracranial pressure monitoring devices.
Role of ICP Monitoring Systems in Managing Brain Disorders
ICP monitors provide crucial information to optimize treatment therapies for various brain conditions. In traumatic brain injury, monitor guides management of elevated ICP levels through therapies like hyperosmolar therapy, sedation or decompressive craniectomy. Subarachnoid hemorrhage patients are continuously monitored for rebleeds indicated by sudden pressure rises. Hydrocephalus management involves shunt surgeries guided by ICP readings post-procedure. Brain tumor surgeries also use monitor to assess pressure changes after tumor removal and detect any complications. Intracranial hypertension in medical disorders can be effectively managed using ICP information from monitors. Overall, continuous real-time data from ICP monitoring improves clinical decision making across range of neurological conditions.
BrainVigil: Intracranial Pressure Monitoring for Neurological Wellness